Glaucoma is a group of eye diseases that gradually steal sight – indeed it is often referred to as the “silent thief of sight,” because most types typically cause no pain or symptoms. Nonetheless, glaucoma is the second leading cause of blindness, after cataracts, and experts estimate that half of the people affected by glaucoma may not know they have it.
Glaucoma is a group of eye diseases that gradually steal sight – indeed it is often referred to as the “silent thief of sight,” because most types typically cause no pain or symptoms. Nonetheless, glaucoma is the second leading cause of blindness, after cataracts, and experts estimate that half of the people affected by glaucoma may not know they have it.
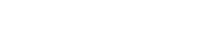
Glaucoma results in vision loss because of damage to the optic nerve. This nerve is responsible for carrying visual information from the eye to the brain. It was once thought that high pressure within the eye, intraocular pressure (IOP), was the main cause of the optic nerve damage. Although IOP is clearly a risk factor, it is now thought that other factors must also be involved because even people with normal levels of pressure can suffer vision loss from glaucoma.
Since there are no noticeable symptoms, glaucoma often progresses undetected until the optic nerve has been significantly and irreversibly damaged, with varying degrees of permanent vision loss. Consequently, early detection is vital to stopping the progress of the disease, and NY Vision Group is dedicated to early and thorough glaucoma screening.
In addition to visual field testing and measurement of intraocular pressure, at NY Vision Group we also monitor for glaucoma with the latest imaging devices of the eye’s optic nerve and internal structures (scanning laser polarimetry (GDx VCC), optical coherence tomography (OCT III), and confocal scanning laser ophthalmoscopy (HRT II). With these advanced diagnostic testing modalities, we can detect glaucoma at its earliest stages often before any vision loss. Additionally, these tests establish a precise baseline measurement of the patient’s optic nerve, which can be reviewed and compared to future tests to detect any changes. This is a key feature to ensure that a patient’s therapy is sufficient to halt the disease.
Types of Glaucoma
Adult glaucoma broadly falls into two categories: Open Angle Glaucoma and Closed Angle Glaucoma.
Open-Angle Glaucoma is the most common form, affecting over 3 million Americans. It occurs when the eye’s drainage canals become clogged over time. The intraocular pressure (IOP) rises because fluid cannot drain adequately out of the eye. Typically with Open Angle Glaucoma, the entrances to the drainage canals are clear and work properly—the clogging problem occurs further inside the drainage canals (similar to a clogged pipe below the drain in a sink).
Most people with Open-Angle Glaucoma have no symptoms and no early warning signs—this type of glaucoma develops slowly and sometimes without noticeable sight loss for many years. There is no cure for this type of glaucoma, however, it usually responds well to eye drops, especially if caught early. Surgical treatment, such as the Selective Laser Trabeculoplasty (SLT), can also slow or prevent further vision loss.
SLT
With SLT a laser treatment is applied to the trabecular meshwork in the eye. This treatment induces biological changes in the drainage system of the eye so that fluid can drain more effectively. Because fluid can drain out, eye pressure is lowered. An SLT treatment takes only a few minutes and is typically performed as an in-office procedure. It is safe and FDA-approved, and clinical trials have shown strong evidence of its effectiveness in reducing eye pressure in most glaucoma patients.
There is no cure for Open-Angle Glaucoma, the most common kind of glaucoma. However, eye drops and laser treatments can slow or prevent further vision loss. At NY Vision Group we are committed to early detection and halting the progression of this disease.
Closed Angle Glaucoma is also known as Acute or Narrow Angle Glaucoma. This type of glaucoma is much less common than Open Angle Glaucoma and differs in that the eye pressure usually rises very quickly. This happens when the drainage canals become blocked or covered over (like a sink with something covering the drain), trapping excess fluid in the eye.
With Closed Angle Glaucoma, the drainage canal is not as wide and open as it should be. The front eye chamber of patients with this type of glaucoma is crammed because then the lens behind the iris is blocking the flow to the eye’s drain and directly narrowing the drain. A simple visual exam is used to see if a patient’s angle is normal and wide, or abnormal and narrow.
If the drainage canal is narrow, an in-office procedure called a laser iridotomy can be used to allow the fluid to get to the front eye chamber, reducing the possibility of a sudden glaucoma attack. During this procedure, a small hole is made in the iris to allow intraocular fluid to travel past the iris to the angle (drain) of the eye. For this type of glaucoma, this laser treatment is usually successful and long-lasting. Over time the eye pressure can still creep upward, as the lens directly continues to worsen drain narrowing. This is resolved in most cases by lens removal (cataract surgery).
Laser Peripheral Iridotomy (LPI)
For patients with Closed or Narrow-Angle Glaucoma, Laser Peripheral Iridotomy (or LPI) is an option. With Narrow Angle Glaucoma, the eye’s drainage canals become blocked or covered over (like a sink with a cover over the drain). This condition is much less common than Open Angle Glaucoma and differs in that eye pressure can rise very quickly.
A Laser Peripheral Iridotomy is a laser treatment that attempts to open alternative pathways for fluid to drain from the eye and prevent more serious glaucoma disease. The angle is the part of the eye that drains fluid from the eye and if it becomes narrowed, the eye is at risk for an acute attack of angle-closure glaucoma. During the procedure, a small hole is made in the iris to allow intraocular fluid to travel past the iris to the angle (drain) of the eye. For this type of glaucoma, this laser treatment is usually successful and long-lasting. However, over time, the eye pressure can still creep upward, as the lens directly continues to worsen drain narrowing. This is resolved in most cases by lens removal (cataract surgery).
Glaucoma Risk Factors
Some people are at greater risk for developing glaucoma and should see their ophthalmologist on a regular basis, specifically for glaucoma testing.
Risk Factors for glaucoma include:
- Age
- Family History of Glaucoma
- Farsightedness or Nearsightedness
- Past Eye Injury
- African or Hispanic Ancestry
- Elevated Eye Pressure